Viruses can infect the brain, hide out for decades, and then cause Viral Parkinsonism
How do you study a disease that takes decades to reveal itself? In this case, scientists used mice, viruses, and a little immunotherapy
In recent years, a mysterious surge of a Parkinson's-like disorder spread around the world, causing an estimated 10-15% of the ten million worldwide Parkinson's Disease diagnoses , baffling doctors and stunning scientists. For years, no one had any idea where the disease was coming from.
Many of these patients were survivors of viral diseases that had infected the brain and led to viral encephalitis. Viral encephalitis is brain swelling and damage, which can occur when a virus infects the central nervous system and ends up in the brain, a condition which can be disabling and often fatal. In fact, nearly every Spanish Influenza patient who had an acute episode of encephalitis (brain swelling and damage during infection) from the influenza virus went on to develop what was later termed "Viral Parkisonism". Epidemiologists have determined that Spanish Influenza survivors have a 2-3x higher risk of developing Parkinson's Disease, now termed Viral Parkinsonism, compared to those who did not come into contact with the virus. Since this time, viruses like the West Nile Virus, HIV, and Western Equine Virus have all been attributed to Viral Parkinsonism development later in life.
Viral Parkinsonism is a disease of neural degeneration from a viral infection that causes encephalitis, or brain inflammation. The strange thing about this illness is how long the delay between infection and disease can be, throwing off a doctor's diagnosis (it's hard to diagnose a cause when it occurred decades before symptoms). There are Parkinson's-like symptoms such as loss of motor control, stiff movements, and loss of balance or difficulty walking. These symptoms arise in eerily high rates post-viral-infection, including in more than 50% of West Nile Virus survivors and nearly 25% of Western Equine Encephalitis Virus patients in a recent Colorado epidemic. But what causes this development of brain damage and its late onset remains a mystery to scientists and doctors alike.
Researchers Colin Bantle and colleagues primarily from the Department of Environmental and Radiological Health Sciences at Colorado State University, USA, set out to address these gaps. They published their findings in 2019 in the npj Parkinson's Disease journal. They were interested in Viral Parkinsonism caused by Western Equine Encephalitis Virus (WEEV), one of many viral infections known to cause encephalitis. WEEV is transmitted by mosquitoes, and can cause disease in a number of hosts including humans and horses. The worst WEEV outbreak recorded occurred in 1941, with over 3,000 confirmed human cases on record. In the last 50 years, approximately 700 symptomatic cases have been reported in the USA alone, with twice as many women as men affected.
Bantle and colleagues were able to show that WEEV delivered through the nose of lab mice could cause 100% lethality in the mice. They then prevented this high mortality by introducing immunotherapy in the form of serum to allow the mice to recover. Serum isolated from blood of recovered animals carries antibodies to infection, which can help an animal fight off an overwhelming viral infection. This animal model now serves as a mimicry of human infection and recovery from WEEV. This could solve the animal model barrier for future research of a variety of disorders, including Viral Parkinsonism, Parkinson's Disease, and many others.
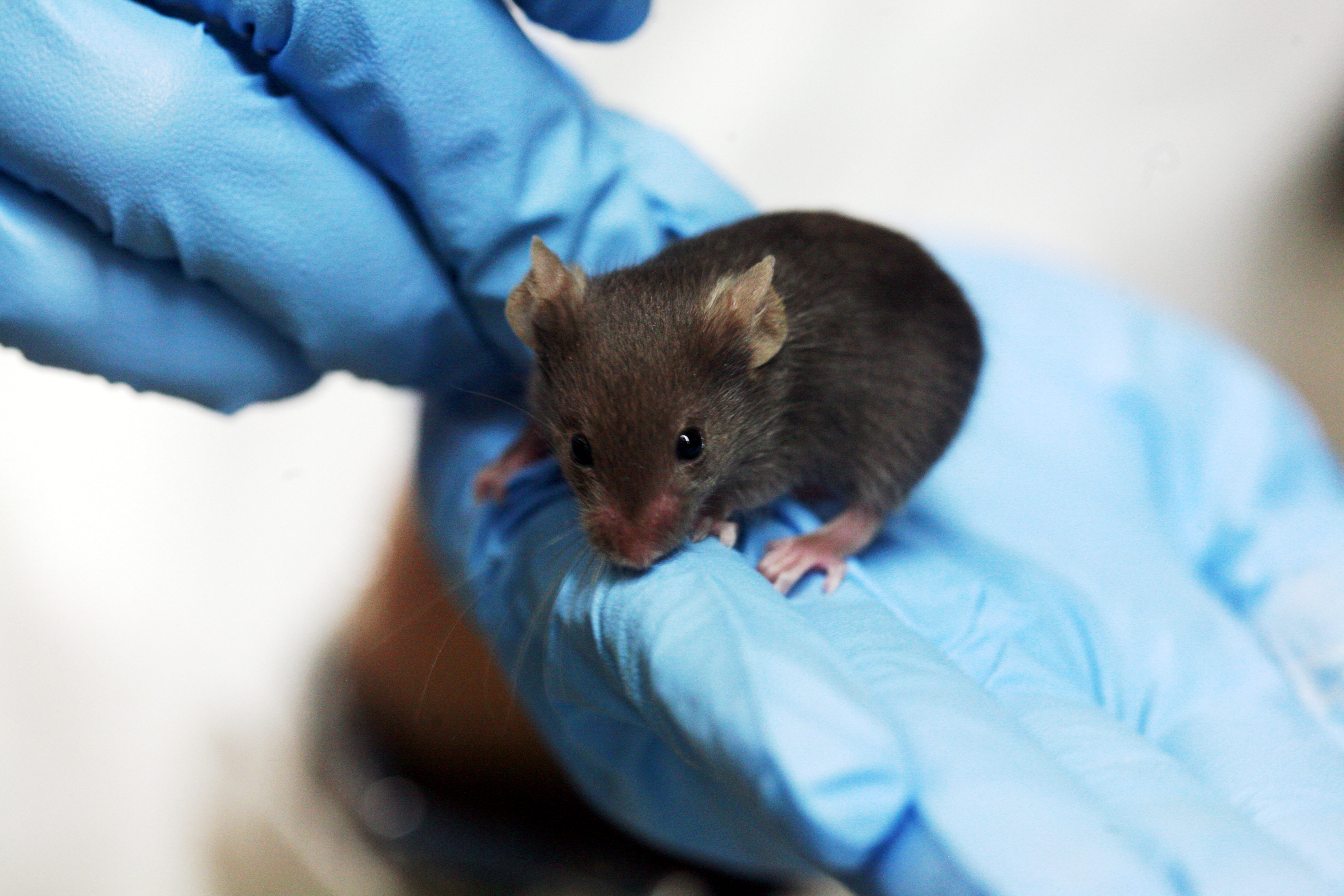
These little mice could hold the answers to how Viral Parkinsonism can arise from a viral infection.
Rama on Wikimedia Commons
Spread of WEEV in the mice was extremely rapid, with untreated mice (those not receiving serum treatment) not surviving longer than 96 hours post-infection. The virus quickly moved from the nose to the brain, where it caused hypokinesia (decreased bodily movement), lethargy (activity decrease due to tiredness), and hunched posture (a symptom of infection and illness in lab mice). A loss of dopamine neurons in the brain was also seen within 4 days of infection, a hallmark of Parkinson's-like neurological dysfunction development.
Brain images of infected mice showed infection of the substantia nigra (an important structure for movement), and ventral tegmental area (the area of the brain responsible for dopamine production and circulation). Loss of dopaminergic neurons (neurons, or signal-transducing brain cells that transmit dopamine) are also a hallmark sign of Parkinson's-like disease progression.

In the USA alone, over 50,000 people are diagnosed with Parkinson's disease each year, where people with Parkinson's include actor Michael J. Fox.
An increase in microglia levels is also a hallmark of Parkinson's-like disease progression. Microglia are a type of immune cell in the central nervous system, and one of the first contacts of invading pathogens, such as viruses. So, an increased level of these immune "superheros" indicate a disease of the central nervous system, including the brain. In this study, Bantle and colleagues found a 31-46% increase in microglia throughout the brain, indicating infection of the central nervous system. An increase in astrocytes (similar to microglia, these are another first-responder immune cell of the central nervous system) was also noted to increase 56-79% in various areas of the brain. What this virus has in common with other Parkinsonism-inducing viruses is that they are all capable of directly infecting the brain, leading researchers to believe that central nervous system viral infections can often to lead to development of a Parkinson's-like disease later in life.
One fact all scientists can agree on is that protein aggregates in the brain, specifically alpha-synuclein aggregates post-infection are almost always present in Parkinson's Disease development. Consistent with previous findings, Bantle et al. also found these alpha-synuclein aggregates in the brains of surviving mice (those that had been infected with WEEV then treated with serum immunotherapy).
The first is the new potential mouse model for study of Viral Parkinsonism. Researchers were able to stimulate disease symptoms in mice exclusively in the brain. This strengthens the model for research, as widespread disease would be difficult to study (when everything is infected, it's hard to narrow down results to a specific area and function, in addition to the fact that Viral Parkinsonism is seems to be stimulated by encephalitis, which is exclusive to the brain).
The researchers suggest that the increased number of immune cells in the brain could promote inflammation, causing more damage post-infection, also potentially leading to Viral Parkinsonism. The final findings together suggest that the loss of dopamine-producing nerve cells combined with alpha-synuclein aggregates from the viral infection partially explain how encephalitis from a virus can lead to Viral Parkinsonism later in life.
Though we know there is a connection between these viral infections and disease progression decades later, many mechanisms remain unknown. However, this study suggests a potential new cause of Viral Parkinsonism, and presents a new animal model for future research. In the USA alone, over 50,000 people are diagnosed with Parkinson's disease each year, 10-15% of whom are Parkinsonisms, diseases that share Parkinson's-like symptoms but progress more quickly, a category that includes Viral Parkinsonism. This study could pave the way for future research on how we can prevent encephalitis from leading to future brain disease, restoring quality of life to those suffering from the condition.
Peer Commentary
Feedback and follow-up from other members of our community
Bhavya Singh
Microbiology
McMaster University
This is so interesting - the article was a joy to read! I had no idea that Viral Parkinsonism was so prevalent around the world. I just had one question - since there is often a big delay between infection and disease, and since survivors of viral diseases are more likely to develop Viral Parkinsonism, is there any way to screen for it? Can doctors periodically check up on these survivors to potentially detect markers for disease onset? I suppose looking for protein aggregates is one way?
Monica Javidnia
Neuroscience
University of Rochester
Parkinson’s disease is highly heterogeneous; there are numerous causes and risk factors (many still unknown), differences in which symptoms manifest and how, varying responses to medication, a large range in age of onset, and more. For this reason, Parkinson’s is sometimes referred to as “Parkinson’s diseases”, and the umbrella term for symptoms or conditions that look like Parkinson’s is known as Parkinsonism or Parkinsonian disorders.
As Marnie notes, “How do you study a disease that takes decades to reveal itself?” In a recent Massive Science article, I described the “prodromal” Parkinson’s, the years or decades before the Parkinson’s diagnosis, and how some drug development efforts aim to target that period in hopes of slowing or preventing disease processes. Some researchers also seek to understand specific Parkinsonian disorders or Parkinson’s disease subtypes based on microbiome, etiology, or other factors of interest. To do this well, scientists need solid cellular and animal models that recapitulate the disease. It is quite promising to see the mouse model described in Marnie’s article check so many of the boxes for what we would see in humans, and I’m looking forward to seeing future research with these mice.
I agree with you completely. It’s exciting to see there is some progress in mouse models and potential expansion to animal models in general for Parkinson’s Disease. There certainly are few currently. I hope this relatively new paper is the start of a trend toward more feasible options for animal models for neuronal degradation such as Parkinson’s and other viral encephalitis cases.
I figured that was the case :) Great article!
Sahana Sitaraman
Neuroscience, Behavior
National Centre for Biological Sciences, India
Great article Marnie. You’ve done a thorough job explaining the chronology of the biological events from the start of the viral infection to the manifestation of the Parkinsonism. If I understand correctly, the virus can infect any and all neurons, once it crosses the blood brain barrier. What I don’t understand is why are dopaminergic neurons affected preferentially? Do the patients not display symptoms of other neurodegenerative diseases? And if this is the case, it paves way for more directed pharmacological interventions. Let me know what you think.
Thank you for commenting Sahana. Researchers think that the primary reason why dopaminergic neurons are more susceptible to damage during Parkisnon’s Disease development is because they seem to be more negatively affected by those alpha-synuclein aggregates I mentioned in the article than other types of neurons and brain cells. These protein build-ups seem to affect the intracellular signaling pathways of these neurons more than others and cause more damage, but researchers still are unclear why this is the case. A great question that I hope we’re getting closer to solving!