Drug repurposing gave remdesivir its second, third, and fourth chance
The antiviral has had a charmed life, failing multiple times but coming back again and again
On May 1, 2020, the FDA authorized remdesivir for emergency use on COVID-19 patients, based on "promising results" out of a National Institutes of Health clinical trial.
Three weeks later, a preliminary report published in the New England Journal of Medicine reported that remdesivir had modest therapeutic effects on adults hospitalized with COVID-19, speeding up the median recovery time by 4 days. More recently, a study in Nature that appeared online on June 9 reported that administrating remdesivir during the early stages of SARS-CoV-2 infection was associated with lower virus level and less lung damage in rhesus macaques. Though the rhesus macaque model is imperfect, and "does not represent the severe disease observed in a proportion of COVID-19 patients," the study authors suggested that early remdesivir treatment may prevent the development of pneumonia in patients.
A press release from the FDA, released June 15, based on data from a non-clinical laboratory study warns against potential interactions between remdesivir and hydroxychloroquine that may reduce remdesivir's antiviral activity. Hydroxychloroquine was previously touted by the administration as a COVID-19 treatment despite little clinical support. The FDA revoked its emergency use authorization for hydroxychloroquine in a separate press release, also published on June 15.
The recent flurry of research effort dedicated to remdesivir is a dramatic reversal in fortune. Less than a year ago, the drug was abandoned based on lackluster data from clinical trials. Remdesivir has been granted a rare second chance to do what it couldn’t do for Ebola in the fight against coronavirus.
After the ill-advised frenzy over hydroxychloroquine, and the FDA’s cautioning that it can lead to heart problems, remdesivir emerged as the next experimental treatment for coronavirus. With a coronavirus vaccine 12 to 18 months away under the best of circumstances, the race is on to flatten the curve and slow the spread of the epidemic so that the healthcare system can keep up with the flood of new patients.
Gilead Sciences, Inc., the U.S. biopharmaceutical company that developed remdesivir, has been here before. Designed to treat Ebola and Marburg virus infections, remdesivir (known as GS-5734 during development) rushed through clinical trials after it blocked symptoms in rhesus monkeys infected with Ebola virus. However, by the time GS-5734 saw compassionate use, the worst of the 2013-2016 West African Ebola virus epidemic had passed, hampering further wider testing.
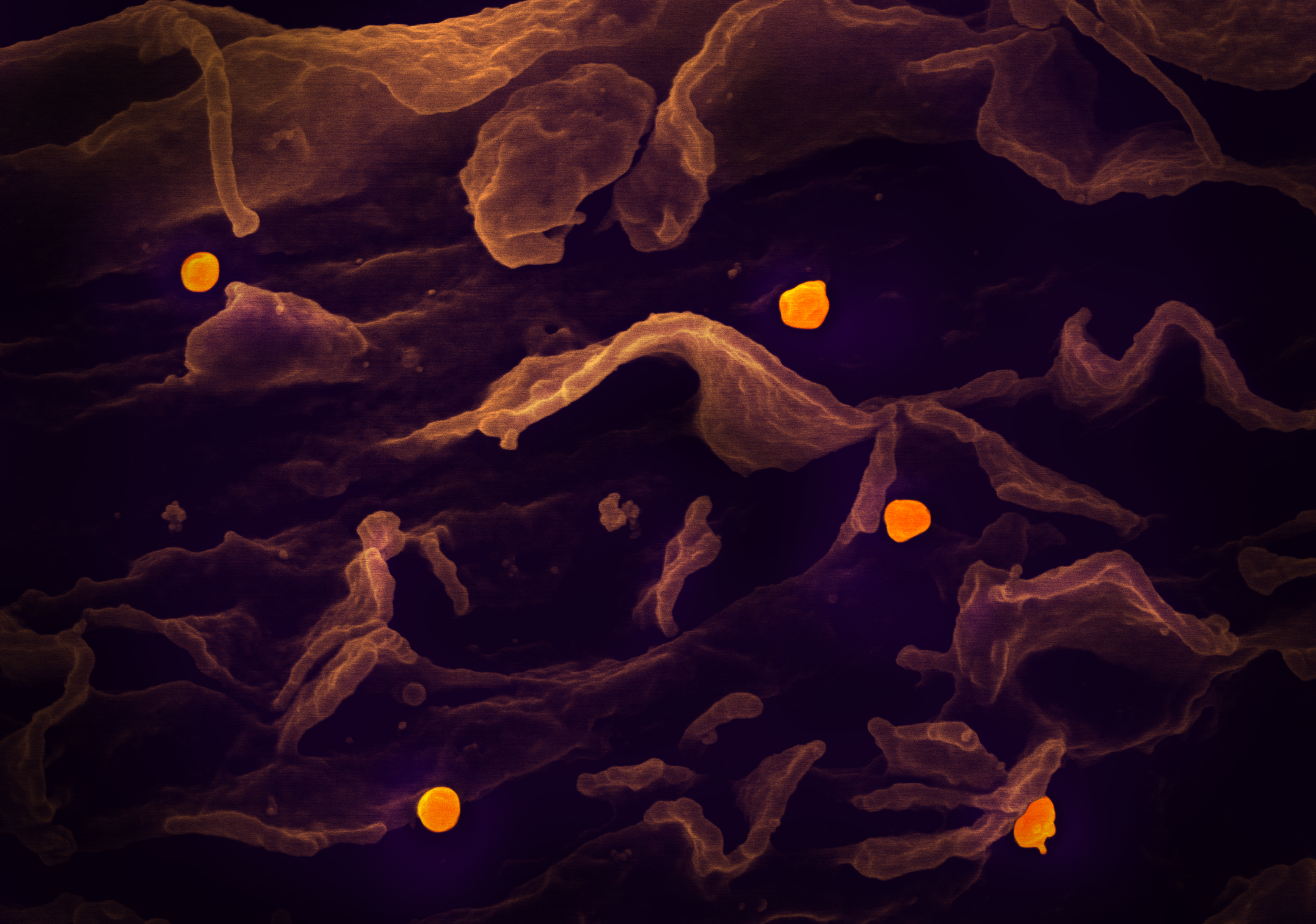
Nipah virus (orange), which remedesivir has also been tested as a treatment for, in African green monkeys
National Institute of Allergy and Infectious Diseases, NIH
A 2018 Ebola outbreak in the Congo became GS-5734’s new testing ground. The treatment ultimately failed in the field – in August 2019, it was dropped from clinical trials after it was less effective at improving survival rates than two monoclonal antibody therapies.
The remdesivir story could have ended there, another victim to the difficulties of translating basic research to clinical applications. But bringing a new drug to market is expensive, routinely taking years of work and costing billions of dollars, so there’s a huge incentive to get something out of failed drugs to recoup the sunk costs of research and development.
One way to do this is drug repurposing, the practice of deploying old drugs for new therapeutic uses. This appears to be Gilead’s strategy in the years following its late deployment during the West African outbreak.
A 2017 study, funded by the CDC, demonstrated remdesivir’s antiviral activity against several families of viruses in cell culture, prompting the authors (who were Gilead employees) to “support new indications for this compound against human viruses of significant public health concern.” Though it is not approved for any indication (other uses), GS-5734 quickly gained a reputation as a broad-spectrum antiviral.
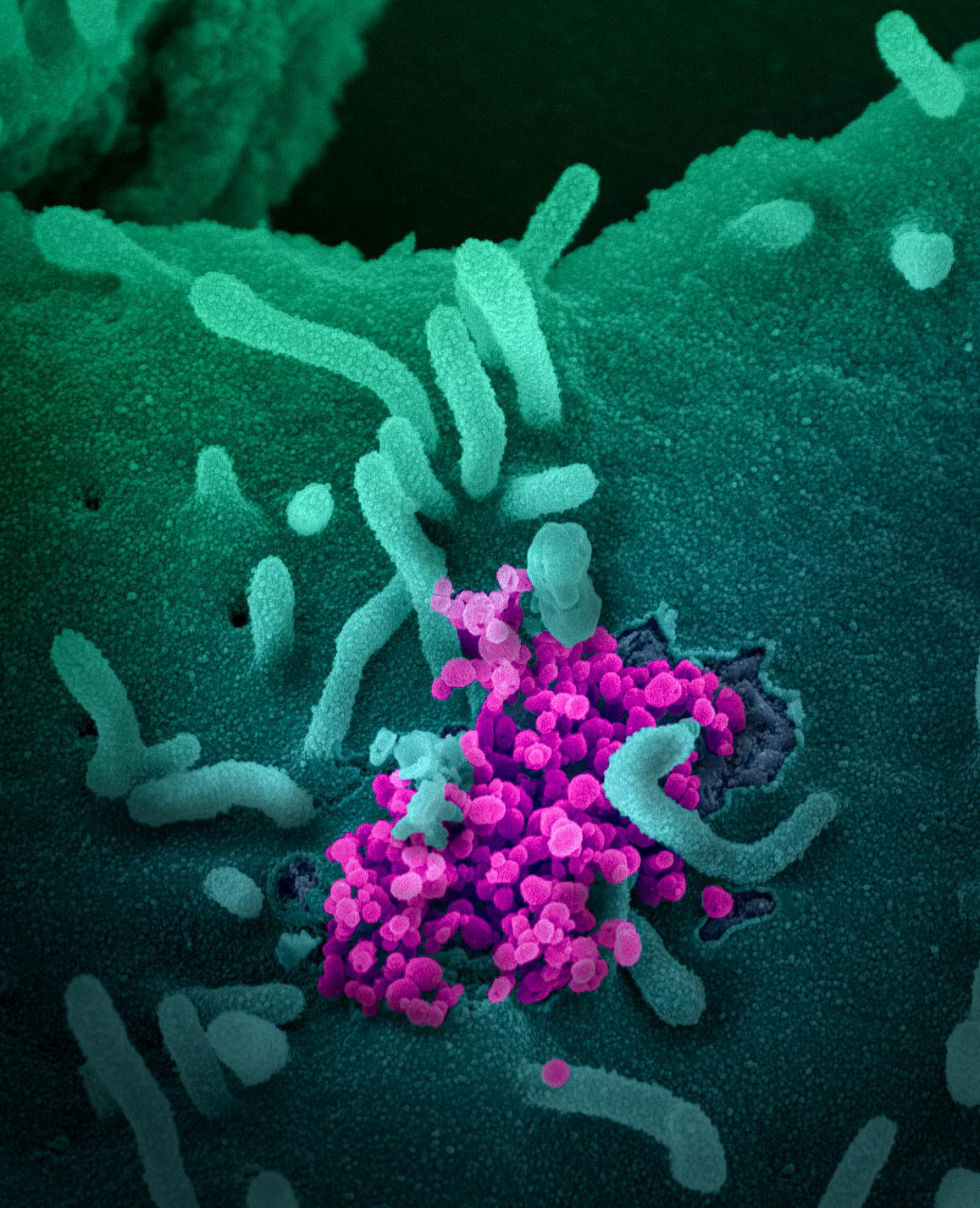
SARS-CoV-2, coronavirus (magenta), emerging from a cell (green) cultured in a lab
GS-5734 interferes with a virus's ability to replicate, and may speed up recovery from infection, though an accidental release of data from a trial conducted in China suggests results are mixed. Despite this, officials remain hopeful, drawing comparisons to AZT, an HIV drug that also stumbled early on.
Now known by its generic name, remdesivir stars in six ongoing studies for coronavirus treatments, including two Phase 3 clinical studies to evaluate its safety and efficacy in adults diagnosed with moderate and severe cases of coronavirus disease.
Clinical trials, when done properly, are a time-consuming gauntlet. The safety and efficacy of a potential new therapy are relentlessly evaluated to determine the optimal dosage, its interactions and side effects, and other key characteristics in a series of increasingly stringent clinical trial phases. Only after passing Phase III trials is a drug eligible for FDA approval, a critical step in its indication to treat a specific medical condition.
Fewer than 10% of drug that start clinical trials make it to launch, and that comes after years of basic research into a compound’s chemistry and toxicity. Remdesivir’s history as an Ebola drug gave it a leg up from novel compounds, because there was already clinical data about its safety profile.
Failed drugs aren’t always a dead end. Drug repurposing attempts often fail, and its occasional success, like the angina drug sildenafil (Viagara, now used to treat erectile dysfunction) or the disastrous morning sickness pill thalidomide, now used to treat leprosy and some cancers, are legendary.
The next "big cure" may already exist, languishing in the pages of an obscure journal or forgotten in stacks of data from a forgotten clinical trial.
Peer Commentary
Feedback and follow-up from other members of our community
Josseline Ramos-Figueroa
Chemical Biology
University of Saskatchewan
Beautifully put! I am somewhat familiar with this topic. Repurposing drugs seems to be the most viable way to find answers in the shortest amount of time possible; the only limitation is finding the right spot where to look, for example drugs that have passed phase I clinical trials or ones with known mechanism of action. Although remdesivir is promising and this is certainly exciting, I wonder about the resulting cost of this drug and how accessible it would be for the population in developing countries. To consider this aspect, I wish more investment on repurposing cheap and more accessible drugs could be done. But like you mentioned, repurposed drugs often fail and we might be still a long way to go.
Fanni Daniella Szakal
Marine Biology, Science Journalism
Interesting article! Drug repurposing is certainly an efficient way of coming up with new therapeutics in a short time. There are quite a few drugs on trials right now against COVID-19 that were effective against other coronaviruses, so new developments will hopefully be coming soon. As for remdesivir in particular, following up on what Josseline mentioned, accessibility is a big issue. If I’m not mistaken, it seems that most of the supply has been bought up until the end of September to be used in the US exclusively. While there are some companies starting to produce a generic version, such as Mylan in India, the drug will most likely be unavailable in most countries for a while at least
Sara Wong
Neuroscience
University of Nottingham
I do think drug repurposing is handy, especially with the situation we are in now. New drugs often fail in regards to safety, so using a drug that is already known to be somewhat well accepted, or one that we already know more about saves so much time than starting from scratch! I do wonder though, how remdesivir compares to dexamethasone, and the possibility of using them as a combo since they possess different mechanims…