Scientists are recruiting live bacteria to fight deadly infections
A study in rural India is raising hopes for a future without antibiotics
The state of Odisha (formerly Orissa) in southeast India is perhaps not the first place you’d expect to find a clinical trial for a next-generation drug with the potential to save half a billion lives. A largely agrarian province, over 80 percent of Odisha’s inhabitants live in small, rural communities and earn, on average, $1.50 a day. Consequently the state has a higher-than-average mortality rate, and an infant mortality rate of 65 per 1,000 live births, double the world average.
And yet, from 2008 to 2012, 4,500 women and their newborns there participated in a potentially game-changing study testing a new treatment for infant sepsis – a study whose recently published results just might hold the key to a post-antibiotic future.
Sepsis kills approximately a million newborns globally every year, but we still don’t know much about how it works. The CDC defines sepsis as “the body’s extreme response to an infection,” a remarkably vague definition for such a lethal disease. So far there’s only one real treatment for sepsis: antibiotics . But the world is fast running out of them. This is because as doctors keep prescribing antibiotics indiscriminately, more and more bacteria, including the ones that cause sepsis, are becoming resistant to them. To compound the problem, big pharmaceutical companies have pulled money from antibiotic research. All of this led UN secretary general Ban Ki Moon to declare antibiotic resistance a "fundamental threat to global health". A recent Indian study also found a scarily high degree of antibiotic resistant bacteria in newborns suffering from sepsis.
'Helpful' bacteria
Fortunately, the Odisha study’s recent results point to a non-antibiotic, affordable treatment that can reduce newborn deaths caused by sepsis by an astonishing 40 percent.
Unhelpful, helpful, very unhelpful
This treatment is a concoction of live, "helpful" bacteria (called probiotics) and a plant-derived sugar (called a prebiotic) that serves as a nutrient source for these bacteria to feed upon. For this study, a team of Indian and American researchers used this synbiotic formulation to treat newborns, and found that the treatment lowered the occurrence of a variety of illnesses: three kinds of sepsis, diarrhea, and infections of the umbilical stump.
While reductions in these diseases were expected, even the researchers were surprised to find that feeding live bacteria to infants also reduced their chance of acquiring pneumonia. The trial was so successful that the the group, led by University of Nebraska Medical Center epidemiologist Pinaki Panigrahi, terminated it ahead of time, a measure undertaken only when the results of a clinical trial are so striking that it is unethical to keep enrolling participants in the control group.
More milk, please
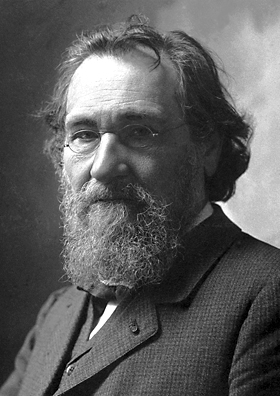
Photo via Wikimedia Commons
This idea of treating diseases through the ingestion of live bacteria was originally proposed in 1907 by a Russian Nobel Prize-winning scientist, Ilya Metchnikoff. His theory went that we could treat serious ailments by replacing harmful bacteria living in our guts with more beneficial ones. While Metchnikoff stretched his theory to dubious conclusions (he drank sour milk every day in the hope that he could delay aging!), the idea has been revisited in recent years as scientists have started to gain a better understanding of what we now call the human microbiome – the millions of bacteria we carry around with us, in our guts, our mouths, and even on our skin. And they've found that using it in treating premature infants and newborns is especially efficacious.
The Odisha study stands out, however, for two reasons. It is the first study to report such positive results in full-term newborns. This expands the patient range for probiotics well beyond premature births to a much larger proportion of the global population. More importantly, it serves as a model for future studies into diseases that especially burden low-income countries and regions.
Clinical trials of the latest experimental medicines are often out of reach of scientists, doctors, and patients living in poorer parts of the world. However, even when trials are implemented in countries like India, they are often run unethically – in some cases subjects are denied even the most basic of patient rights: informed consent. According to a recent Indian parliamentary report, the blame lies with everyone involved, from the Ministry of Health to the international funders behind the trials. Even if trials go well, most new, patented, drugs are prohibitively costly, even by the standards of developed countries, they hence remain off-limits to the very patients they were tested on.
A counter-example to model
The Odisha study, to my mind, is an ideal counter-example, showing how a successful clinical trial can be held in a poor, under-developed region. The authors (hailing from five US universities and four Indian institutions, and funded by the US National Institutes of Health) describe how they set up an entire trial infrastructure including a three-tier hierarchy of scientists, on-site doctors, 200 volunteers, and government health workers; a network of local hospitals; and an impressive process for interacting with the expectant mothers enrolled in the study (including regular focus-group meetings and video seminars on symptom observation). It is difficult to find estimates of how much a pill of live bacteria and sugar might cost, but according a Dutch report, using probiotics could reduce healthcare costs by up to 25 percent.
As the threat of antibiotic-resistant infections grows ever more real, scientists in labs around the world are experimenting with next-generation anti-microbials ranging from carbon nanotubes to engineered viruses. These are expensive, patented interventions still far from reality.
The Odisha study suggests that the answer, at least for several million newborns, may lie in a relatively cheap, low-tech approach first dreamed up by a Russian in 20th-century Paris, and tested a hundred years later by American and Indian scientists with the help of 4,500 brave Indian women.
Peer Commentary
Feedback and follow-up from other members of our community
Melanie Silvis
Molecular Microbiology
UC San Francisco
This is a very well-timed article that addresses a pitfall of our current dependence on antibiotics.
The most remarkable finding of this paper to me is that treating newborns using probiotics substantially improves their outcomes when they have viral infections. For bacterial infections, I can imagine how beneficial bacteria may outcompete the infecting bacteria to ameliorate sepsis. To have an effect on viral infection is truly wild to me, and leaves me with a few questions:
First, in many cases the cause for sepsis is unknown, and may very well be a viral infection. Obviously antibiotics would be useless in this case, but often doctors have no way of distinguishing bacterial and non bacterial causes of sepsis. The second question needs more research to answer but in trials so far, the best results for probiotics have been seen only in newborns or in premature babies.
Kevin Pels
Chemical Biology
Dana-Farber Cancer Institute
This isn't something you get into in the piece, but it begs the question: what are 'good' bacteria, and why do they 'work'? The specter of bacterial warfare to establish a balance of power is a bit too simplistic, and does little to reveal a mechanism. Fundamentally, either the good bacteria (with their prebiotic noms) are enforcing a healthier phenotype via a positive mechanism, or they are mitigating a less healthy phenotype expressed when the bad bugs reign supreme.
Large-scale microbiome studies have done little to provide classifications at the taxonomic level of which bacteria are good and bad. So to come back to the research, by whatever mechanism, dysbiosis – microbial imbalance – seems to be attenuated, even without that deeper knowledge. I still want to know what's going on with these (Lactobaccilus plantarum) & other 'good' bacteria at the molecular level.
Sukalp Muzumdar
Molecular Biology
ETH Zurich
I think this is a very interesting finding; to me it seems as though two major mechanisms are being proposed for the observed outcome - the tolerization of the intestinal immune system, as well as the competitive colonization of the gut by "beneficial" bacteria.
It would be an interesting follow-up study to use these synbiotics as an adjunct treatment for newborns who have already developed sepsis to show which one of these two mechanisms is more dominant - as immune tolerization should play a much smaller role in this inflammatory condition.
Given that we now have a preliminary preventative treatment for sepsis, I find it difficult to imagine an IRB approving a trial where this treatment is withheld until the babies develop sepsis. It would be easier to test the alternative hypothesis by running a metagenomics screen on fecal matter in patients responding positively to the synbiotic and those who do not see any alleviation.
Well, it would be rather hard to define positive and negative responders unless there were established criteria/biomarkers for this.
Furthermore, I think a 40 percent reduction of risk is not sufficient to bring about the introduction of prophylactic probiotic treatment in countries which have a rather low preexisting incidence of sepsis in term infants (which were the target of this study). In such contexts it would be more interesting to investigate probiotic administration as a replacement treatment for antibiotics.
I disagree – a 40 percent reduction is a huge benefit, and sepsis is a leading cause of neonatal mortality globally. Administering antibiotics and probiotics would make no sense since the bacteria would just die. And maybe you need a more diverse gut flora for the probiotics to act (this could be studied in the lab). Also, in neonates the time for responding to sepsis is quite small, and antibiotics are also not recommended for treating infants so a prophylactic administered at birth sounds like a good idea to me.