Rapid DNA sequencing of unknown bacteria helps doctors choose which antibiotics to treat it with
This could cut treatment time from days to hours and decrease overall antibiotic use
WikiImages on Pixabay
Imagine that someone you know went into the hospital with a bacterial infection. Now imagine that the hospital’s microbiology lab could immediately sequence the genome of the bacteria making them sick. The results would tell their doctor on the fly which antibiotics to use.
This type of personalized medicine may be possible in the near future, thanks to a team of researchers led by Karel Břinda and based at Harvard Medical School and the Harvard T. Chan School of Public Health. The team developed a way to swiftly diagnose bacterial infections, and more importantly identify if the bacteria causing the infection are resistant to antibiotics. Current methods take days for labs to grow the bacteria and test it for antibiotic resistance. This tool could shorten that timeframe from days to hours.
The development is possible thanks to a pocket-sized piece of technology called the Oxford Nanopore MinION. The device, smaller than the average smartphone, can be plugged directly into a computer. In that tiny package it holds all the components necessary to sequence an entire bacterial genome.
This MinION has been used before to sequence and identify culprits of infection, but what makes this study unique is how the researchers analyzed the data. They compared the sequenced pieces of DNA against previously studied bacterial isolates to identify the bacterium’s closest known relative. They called this method “genomic neighbor typing." It’s similar to when a primary care doctor asks about family history to identify if a patient is at higher risk of developing certain diseases. In the same way, knowing which other bacteria the infection is most closely related to allowed researchers to determine the antimicrobial resistance of each individual infection.
This genetic comparison was accomplished using a computer software they developed and cheekily gave the acronym RASE (Resistance-Associated Sequence Elements) for its ability to speedily identify antibiotic resistance.
Traditional ways of diagnosing and treating bacterial infections are very time-consuming. First, bacteria must be isolated from the site of infection. That sample is then taken to a microbiology lab. Each subsequent test requires more time to either grow more of the bacteria (a process called culturing) or run the test. Newer technologies have enabled rapid identification of pathogens, but unfortunately antibiotic resistance testing still requires culturing the microorganism first. Identifying antibiotic resistance can take between 2-7 days.
In the meantime, clinicians have to make rapid decisions about a patient’s care; this often results in the prescription of broad-spectrum antibiotics which are not guaranteed to be effective against an infection. Having antimicrobial resistance information faster would enable doctors to use more targeted therapy, which would result in better patient outcomes. The risks of antibiotic resistant bacteria are serious – the CDC estimates that antibiotic resistant infections are responsible for 35,000 deaths in the US alone every year. And even for patients who recover, infection with a resistant microbe is likely to increase the length of hospital stay and result in higher healthcare costs.
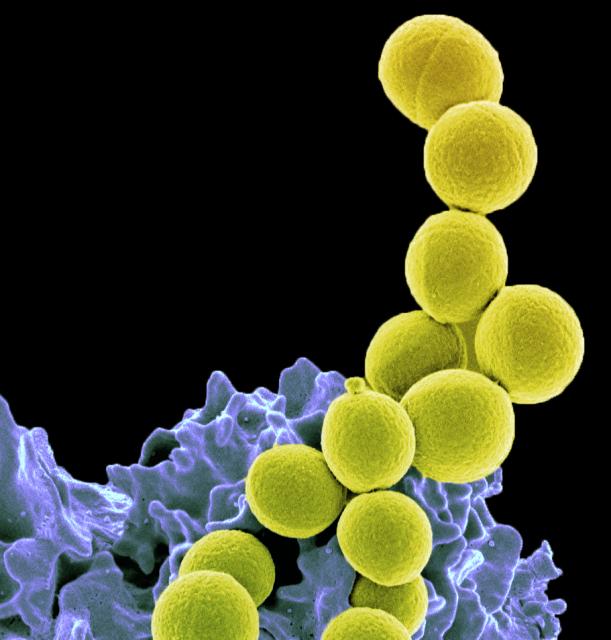
Drug-resistant bacteria
Beyond individual patient care, it is even possible that rapid identification of effective antibiotics could improve antimicrobial stewardship, a worldwide effort to make sure doctors and patients only use antibiotics when necessary, and use them correctly when they do. Exposing bacteria to antibiotics promotes the development of antibiotic resistance. The possibility of using fewer, but better targeted, antibiotics, could help slow the spread of antibiotic resistance and allow doctors to save newer antibiotics for the truly resistant infections.
While this new method shows great promise for rapidly identifying antibiotic resistant organisms, it is far from ready to be implemented in the clinic. So far the researchers have only tested it on two bacterial species on the CDC’s list of biggest antibiotic resistance threats: Streptococcus pneumoniae and Neisseria gonorrhoeae. To be ready for implementation, this method needs to be expanded to include more bacteria that are antibiotic resistance threats. Beyond that, public health agencies around the globe will have to participate in collection and characterization of bacterial infections because this method is only as good as the database of bacterial sequences it has to compare to. If governments get involved and make surveillance of circulating strains a priority, then this tool has the potential to be incredibly accurate.
Another complication that may arise in the hospital is that clinical samples sometimes contain multiple different kinds of bacteria. This is partly due to errors in sample collection and partly because our bodies (which incude our microbiomes) are 1-3% bacteria by weight. Sometimes it is hard not to get some of the microbiome along for the ride when collecting a clinical specimen. This study was tested on individual bacterial isolates, but to be effective in a clinical setting, RASE will have to be able to differentiate between multiple organisms in a single sample.