A smell test can predict whether unresponsive patients will recover
Smell could be the key to predicting recovery paths for people after brain injuries
Živa Trajbarič on Pexels
Our senses are the only way we have to interact with the world around us. It is by using them that we diagnose and treat people after severe brain injuries.
The Glasgow Coma Scale, for instance, takes into account a person’s ability to listen to commands. If they're not able to do that, then their ability to respond to painful touch stimuli is tested. Other neurological tests also rely on some form of interaction, which if not present, usually indicates a coma, or other disorders of consciousness (DOC). Even with more recent technologies, such as brain imaging, the rate of misdiagnosis in DOC patients could be as high as 40%.
Besides the fact that we do not even have a full understanding of what consciousness is, one of the challenges in diagnosing DOCs is that it's difficult to distinguish between people in persistent unresponsive states, and minimally responsive ones (who have inconsistent but present responses). These distinctions are not trivial, as they not only underlie therapeutic strategies, but can also determine end-of-life decisions. Because of this diagnostic conundrum, there is also no current official number of DOC patients, but the estimates are close to the order of hundreds of thousands.
New research by Anat Arzi and colleagues at the Weizmann Institute of Science shows that maybe we were simply not looking at the right sense. The study presents a new technique that might allow us to use the sense of smell as an indicator of consciousness. The scientists took advantage of something called sniff response — basically the way our brain automatically sniffs in response to a certain stimulus. For example, if you open your garbage and there is something spoiled in it, you will almost reflexively reduce the amount of air you inhale. On the other hand, when walking into your favorite coffee shop, you might inhale more than the normal amount of air to take everything in. These responses can be conscious or unconscious, but they usually reflect some sort of situational understanding.
With that in mind, the team of scientists presented two distinct smells (fruit-scented shampoo or rotten fish) to a group of 43 DOC patients, testing them for over 10 weeks. The first few tests were done to determine the patient's level of consciousness based on their sniff response. They found that in patients in an unresponsive state, there was no significant change in their response to either one of the smells, or the blank test (no smell). In patients previously diagnosed as minimally responsive, there was a decrease in volume of air inhaled with the unpleasant smell compared to the blank, measured through a nasal cannula linked to a machine that analyzes airflow.
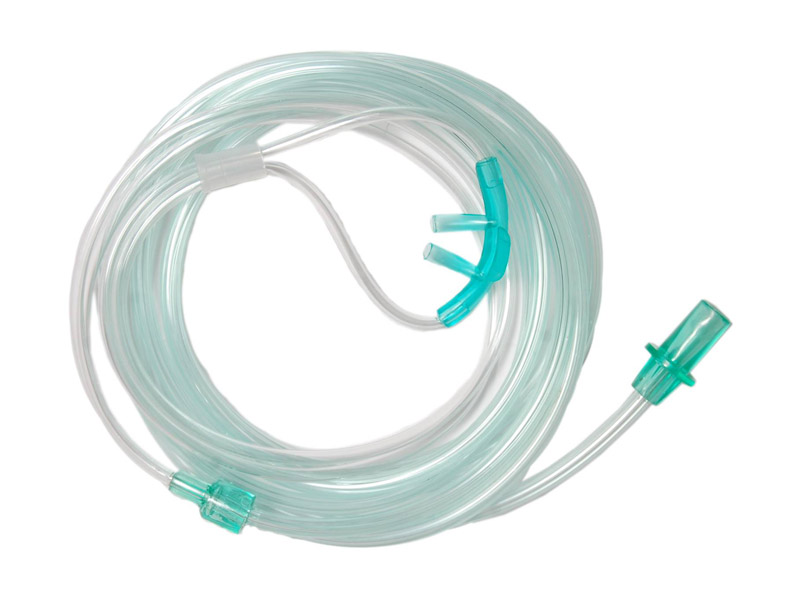
A nasal cannula
Frank Kirby on Flickr
Because they were able to analyze the same patients over time, some of them recovered and some did not. The scientists next examined how the patient’s performance in the sniff test correlated with their clinical outcomes. All of the patients who progressed from an unresponsive state to a minimally responsive state had a positive sniff response in at least one session. That means that there was a strong association between their recovery and their performance on this new test. Even more, in some patients, that sniff response came months before any other sign of recovery. There were, however, false-negatives, or people without a sniff response that also recovered from unresponsive to a minimally responsive state. This happened in 37.5 percent of cases. But this means that in almost two-thirds of the cases, this simple sniff response preceded any sign of recovery.
One important caveat worth discussing is that in many cases, the same injury that caused the damage could affect the brain’s ability to perceive smell. In fact, the team of scientists found that in almost all false-negative patients, there was possible damage to the areas of the brain responsible for smell, shown in brain imaging.
The last test was to see if there was any relation between a patient’s score and their long-term outcomes. About 90 percent of the patients with a positive sniff-response survived the following years, while for the patients without any response that number was closer to 35 percent. Overall, this suggests strong correlations between how DOC patients respond to different smell stimuli, and their diagnoses and outcomes. These are not direct causations, and there is definitely more research needed to turn this into a routine exam, but this new study shows the exciting power that our sense of smell can have.

When walking into your favorite coffee shop, you might inhale more than usual
Photo by Battlecreek Coffee Roasters on Unsplash
There are key limitations, as with any study. One very real possibility was that the patients who recovered were simply misdiagnosed at first. While there is no easy way to test for this, it would be possible to ask recovered patients if they have any recollections from when they were deemed unresponsive, which would indicate a misdiagnosis. Another possible issue would be in the case of a patient who can indeed sense a change of smell, but does not have the ability to inhale because of motor dysfunctions. Although there is no immediate way of testing that, a different study has shown that patients were able to respond to commands asking to control their breathing, but not any other motor functions, which could be further used to distinguish different levels of consciousness.
There is still so much we do not know about our sense of smell and how it relates to our other senses. We know that it is primal and deeply ingrained and integrated with the parts of our brain responsible for memory, emotions, and other higher functions. If used in conjunction with other techniques, such as brain imaging and other clinical assessments, this new test can be a powerful predictor of outcomes for people with severe brain injuries.
Ed: A previous version of this article referred to unresponsive patients as being in a "vegetative state," an ableist and pejorative term that scientists in the field no longer use (for a discussion on this see this article). I regret the error and assume full responsibility. We have added the correct usage to our style guide. - Dan Samorodnitsky, Senior Editor
Peer Commentary
Feedback and follow-up from other members of our community
Shannon Casey
Biology, Medicine
This sounds like an innovative approach toward assessing DOC. The smell test seems quite unreliable at this time, but it’s interesting information nonetheless.
Julia A Licholai
Neurobiology
Brown University
Hi! I think that this - the use of smell tests for neurological issues - is such an interesting topic! I find it fascinating since loss of smell is thought to also proceed neurodegenerative disorders, like Alzheimer’s Disease, and is especially relevant now since one baffling symptom of COVID-19 is the loss of smell. Because the neurons involved in smell, olfactory receptor cells, have a high turnover, people have speculated that there may be ties between developmental genes and neurodegeneration (specifically that impairments of cell proliferation and differentiation in regions with high neurogenesis is believed to contribute to neuronal dysfunction). I wonder if there is a wider relevance of developmental genes to various neurological abnormalities not just for neurodegeneration but recovery in general as seen here.
Nechama F. Sammet Moring
Science Journalism
This is such an interesting story! I’m curious if any follow up research has been done, especially looking at the longer term outcomes, or evaluating what might be enabling people with severe brain injuries to respond to smells? This is so not my area of expertise in any way, but I’ve read some stuff about the connection between scent and memory, for example people with Alzheimer’s who are more able to connect with the world when they are given familiar scents, or the research showing that if you wear a particular scent when studying and then apply it right before taking the test, you do better than people who simply studied, without the smell. It would be really interesting to see research that gave patients with DOC familiar scents from prior to their brain injuries. I wonder if this would also be comforting to patients? There’s so much we don’t know about the brain and consciousness, and this is a fascinating piece of the puzzle
From what I have seen there’s nothing so far based on that study, a few reviews and articles have cited it, and the group published a different story regarding smelling and COVID, but nothing new on DOC yet.
This is just scientific speculation from now on, so take it with a grain of salt, but I think that smell overall as a sense is just recently been given the deserved attention. You might have heard it before how smell does not go through the thalamus, the relay center of the brain, going from your nose to the olfactory bulb and connecting directly to either memory areas or the cortex. This is a possible explanation as to why we have such vivid and quick memories or feelings with smells - before we even realize what it is. It could also be why there is such a strong connection with consciousness. I particularly do not like the whole metaphor of reptilian brain/mammalian brain but in that same idea olfaction is one of the oldest senses from an evolutionary perspective, so it makes sense that it is so essential and so deeply encoded in our consciousness.
Unfortunately, when speaking of Alzheimer’s in particular, these smell tests might not be very effective. Although there is still so much about AD we still do not know, but it seems like anosmia, i.e. losing the sense of smell might be one of the earliest signs of neurodegeneration.
There’s so much we still do not understand about olfaction and about how it connects back to all kinds of facets of our daily experience, so I am particularly excited to follow this group, they are the ones doing some of the coolest research.