Can better sleep help protect us from trauma?
A new study suggests REM sleep may make us less vulnerable to PTSD
What if we could predict who is susceptible to post-traumatic stress disorder (PTSD) before a traumatic event triggers it? A paper published in the Journal of Neuroscience this year suggests that predicting vulnerability or resilience to stress may, in fact, be possible – by examining how people sleep.
The study, by Rutgers University memory researcher Itamar Lerner and colleagues, found that people who spend more time in rapid eye movement (REM) sleep had reduced fear-related brain activity in response to an emotional learning task. These findings suggest that getting enough REM sleep prior to a stressful orscary experience may make a person less prone to developing PTSD.
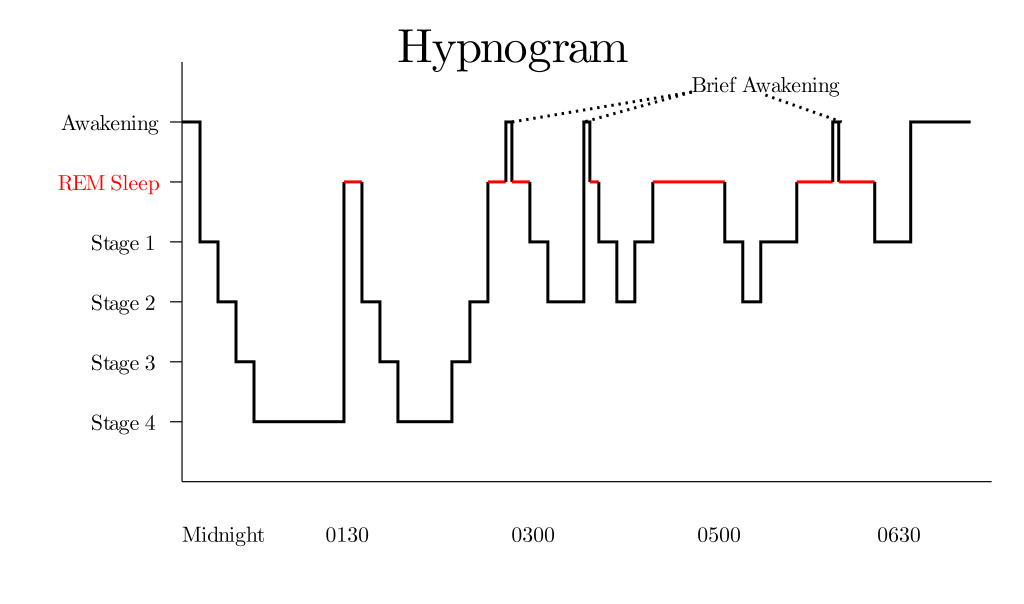
This hypnogram shows the transition between sleep stages between midnight and 6 A.M. Periods of REM sleep are highlighted in red.
Diagram by RazerM via Wikimedia Commons
The brain naturally cycles through five distinct stages of sleep each night: stages 1, 2, 3, 4, and REM sleep. REM sleep makes up approximately 25 percent of your sleep cycle. It first occurs about 90 minutes after falling asleep. During REM sleep, as the name suggests, your eyes move rapidly from side to side behind closed eyelids. Interestingly, brain wave activity closely resembles that seen during wakefulness during REM sleep, and dreams also occur predominantly during this stage.
Now, the role of REM sleep in memory has been discussed for a long time. For example, research indicates that REM sleep is critical for the transfer of emotional memories from short term to long term storage. Moreover, sleep disturbances are one characteristic of PTSD. Specifically, research has shown that PTSD is associated with fragmented REM sleep. What Lerner and colleagues’ study suggests is that these alterations in REM sleep may actually exist before the trauma occurs, and not as a result of the disorder.

Counting humans
Francesco Gallo / The Met
These findings beg the question: can we get better at sleeping to protect ourselves from trauma? Well, one study found that napping diminishes physiological and emotional responses to repeated presentations of fear-provoking pictures. However, the Rutgers study suggests that what we really need is more time spent in the REM stage of sleep. While the best way to increase the amount of time in REM sleep is to get more total sleep, melatonin supplementation has been shown to increase REM sleep in particular.
Fear learning
Lerner and his colleagues concluded that sleep may protect against trauma by examining how baseline levels of sleep effect measures of fear learning. Fear learning, or fear conditioning, is a behavioral model in which subjects learn to predict aversive outcomes. It's often used to understand PTSD. In this study, they first sent 17 subjects, recruited from Rutgers University and the New Jersey Institute of Technology, home with sleep-monitoring devices – headbands that monitored their brain waves – and asked them to sleep normally for a week. During this week, the researchers tracked how much time they spent sleeping and which stages of sleep they spent the most time in.
Next, the researchers conditioned the participants to fear images of rooms lit with differently colored lamps by pairing mild electric finger shocks with some of the colored lamp images. Through these procedures, participants were taught to fear the rooms that were lit by certain colors, but not others. Believe it or not, these methods aren’t as crazy as they sound. For nearly 100 years, in both animal and human research alike, researchers have been pairing cues together to investigate how we learn. While fear conditioning procedures used in people today are rather mild and do not result in any long-term phobias of, for instance, a colored lamp, it does allow researchers to examine markers of fear learning.
One such marker is brain activity. Researchers found that those participants who spent more time in REM sleep had less connectivity between their amygdala (the fear center of the brain) and the hippocampus (the memory center of the brain). They also found a similar association between less time in REM sleep and decreased connectivity between the hippocampus and ventromedial prefrontal cortex (an area of the brain important for coping with stress). Additionally, this study suggested that the less REM sleep the subject had, the higher their physiological arousal was in response to the fear-provoking stimulus.
Then, the Rutgers researchers sought to replicate their finding by recruiting another 17 subjects from the surrounding universities and measuring their sleep patterns, fear learning, and brain activity. The main difference between this and the first experiment was that the subjects’ sleep was only measured for one night before the fear learning task. Again they found that more time in REM sleep was associated with less connectivity between the amygdala and hippocampus.

These studies aren’t without their limitations: the second study was unable to replicate the finding of reduced connectivity between the hippocampus and ventromedial prefrontal cortex in those with less REM sleep. Also, the sample size was relatively small in both experiments, which perhaps contributed to the non-replicated results.
If future work confirms the findings, Lerner and colleagues’ research could have important real-world applications. The development of noninvasive biomarkers of stress resilience or vulnerability may one day influence who we choose to send to war, for example. But, in the meantime, researchers need to continue investigating this link between REM sleep, trauma, and resilience.
Peer Commentary
Feedback and follow-up from other members of our community
Jack Barton
Cognitive Neuroscience
University of Manchester
This is a great article about some very interesting research. The link between REM sleep and emotional memories is fascinating, and it’s encouraging to see that the amount of REM sleep might act as a biomarker for reactivity to fearful situations. As you say, there are some clear implications if the science behind this can be understood further.
The paper in question also highlighted that the link between REM and trauma might be trait-based (e.g. how much time people normally spend in REM sleep over weeks rather than just a single night). In study one, one single night’s REM was not predictive of the observed brain activity changes; however, the average of the week was. This suggests that if modifying REM is possible as a vaccine against trauma then it needs to be maintained to be effective – a habit for more REM rather than a one-off boost.
It would be useful to know whether those with “less REM,” however that is defined, are at a greater future risk for developing PTSD. You could follow up a low and high REM group over many years and assess whether REM does confer some protective ability in a real-life setting. I don’t know of any research that has looked at this yet, but it seems to me to be a great way to move this research forward.
I’ll be restrained but there’s even some work questioning whether sleeping directly after a trauma is such a good thing... I’ll keep a lid on the excitement – for now at least.
Michael Graw
Oceanography
Oregon State University
This is a really intriguing study with a lot of promise for understanding PTSD risk, but I think it's important to add some level of caution to the idea of using REM sleep as a "biomarker" to predict risk. Nearly every study that looks finds a connection between some lifestyle or psychological factor and PTSD risk, both before and after the traumatic event, indicating that low levels of REM sleep is likely only a small piece of the actual predisposition to developing PTSD. That said, the finding that REM sleep is tied to the connection between the amygdala and hippocampus is in itself suggestive of a broader neurological mechanism at work; looking more deeply into that could begin to tie together some of the seemingly disparate threads of PTSD risk.